
Asthma is one of the most common long-term health conditions, so why does access to diagnosis and treatment still depend on where you live, who you see, or even your ethnicity?
To mark World Asthma Day, we spoke with Carol Stonham MBE, a leading respiratory nurse, about what true accessibility in asthma care looks like and why we are not there yet.
The postcode lottery of asthma care
Asthma is a condition where we see a variation of care for many reasons; it’s vital that people with asthma symptoms have access to a quick and timely diagnosis, and those with an existing asthma diagnosis should have equal care, regardless of where they live and who their healthcare provider is. Access to a simple Fractional exhaled Nitric Oxide (FeNO) test is limited in some areas, meaning patients must travel out of their way to take this quick and easy test.
When it comes to care, one size doesn’t fit all, so it is important that care is adjusted to people within the local area. We are working towards a neighbourhood delivery of healthcare and planning services on a neighborhood basis to ensure that care is tailored to the local population.
Why FeNO testing is a game-changer
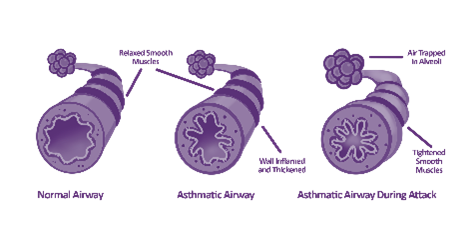
Asthma causes airway inflammation; more nitric oxide (NO) is produced when airways are inflamed. A FeNO test measures NO levels; a high FeNO level suggests airway inflammation and aids an asthma diagnosis but also guides healthcare professionals on their next steps in treatment.
The most recent guidelines for asthma care and management from the National Institute of Health and Care Excellence (NICE), the British Thoracic Society (BTS), and the Scottish Intercollegiate Guidelines Network (SIGN) now recommend a FeNO test as an initial test for diagnosis and asthma management. A FeNO test is quick, easy to use, and fits within a typical 10-15-minute consultation.
Barriers beyond geography
Healthcare professionals (HCPs) and patients must have the correct education. Unfortunately, there is no baseline level of asthma training for HCPs. Without training, it may be challenging to recognise worsening asthma control or inappropriate treatment. If the HCPs have the correct education, patient education will follow nicely; once patients understand their asthma, the treatment and how it works, they will be empowered to manage their condition better and, more importantly, understand when they need to seek help if things are not going well.

In the UK, patients in the lower social economic groups do not access healthcare, so it is more difficult for them to get information and testing. Some may be on the cusp of receiving free prescriptions, but then comes the issue of affording the medication. Some ethnic groups see long-term health conditions as a weakness, so it is vital to get messaging and education out to these communities.
The future vision

The biggest challenge in accessibility to FeNO testing for asthma care is funding; who pays for it? The Integrated Care Board (ICB) will pay for it in some areas, but this isn’t the case everywhere. In some places, it is down to the Primary Care Network (PCN); however, if they do not deem it a priority, it comes down to the individual General Practice (GP) surgeries. We need a strategy across the board where the ICBs take responsibility and ensure the funding is available for their area.
We cannot implement what the new NICE/BTS/SIGN guidelines are telling us to do without access to FeNO testing. Hence, we need to work with the campaigning organisations to demonstrate the full cost-effectiveness of FeNO testing. It would be great to get a system like the one they have in Gloucestershire, where a local enhanced fee is paid for each diagnostic test, meaning the payment received for every diagnostic test goes back into paying for FeNO testing consumables.

Asthma care should not be a guessing game, but without access to the right tools, that is exactly what it becomes.

Want to know how Gloucestershire is a model of accessible care? Or Carol’s expert insights? Watch the full interview here.
